How to Read Your Blood Test Results
Share
Blood tests are a key tool for understanding your health. By learning how to interpret your results, you can spot changes early, make informed decisions, and have better conversations with your doctor. Here's a quick breakdown:
- Reference ranges: These show what's normal for most healthy people. Results outside these ranges may need attention.
- Common units: UK reports use mmol/L for glucose and cholesterol, g/L for proteins, and U/L for enzymes.
-
Key markers:
- Cholesterol: Total cholesterol should be below 5.0 mmol/L; LDL (bad cholesterol) below 3.0 mmol/L.
- HbA1c: Reflects blood sugar levels over 2–3 months. Below 42 mmol/mol is normal; 48 mmol/mol or higher indicates diabetes.
- Full Blood Count (FBC): Checks haemoglobin, red and white blood cells, and platelets to detect issues like anaemia or infections.
- Liver and kidney tests: ALT, AST, and creatinine levels assess organ function.
- Doctor comments: Look for notes like "normal", "abnormal", or "repeat test required" for guidance.
Tracking trends over time and understanding your personal health context (e.g., age, gender, lifestyle) is just as important as the numbers themselves. Always consult your doctor for advice tailored to your results.
How To Understand Your Blood Test Results | Dr. Eric Debunks
How to Read Your Blood Test Report
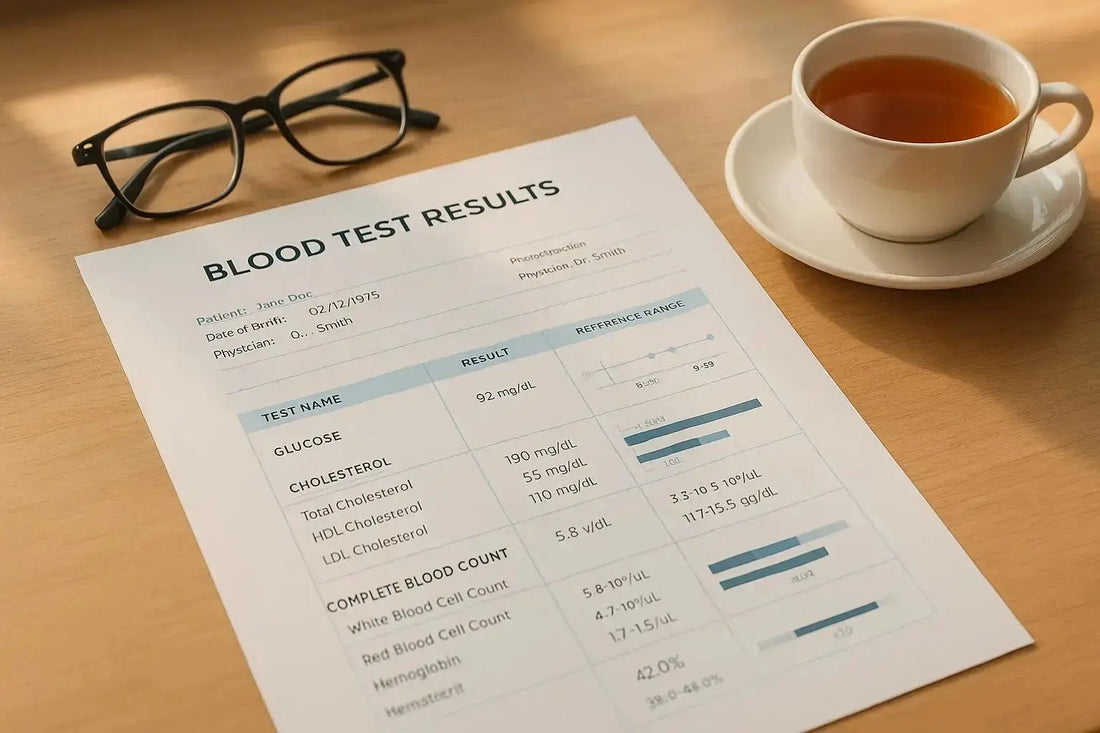
Blood test reports might seem overwhelming at first glance, but they generally follow a standard format that becomes easier to understand with a little guidance. Whether you're reviewing a report from the NHS or a private lab, the layout is usually similar, helping you track your health and have informed discussions with your doctor.
The report typically begins with your personal information and the date your sample was taken. Following this, you'll find a list of the tests performed, each accompanied by your results, the reference range (normal values for healthy individuals), and the measurement units used. There may also be comments from the lab or your doctor, offering additional context. With this framework in mind, you can interpret your results more confidently.
What Reference Ranges Tell You
Reference ranges show the typical values found in 95% of healthy individuals for each test. These ranges, often displayed in brackets or a separate column, can vary depending on factors like age, gender, and sometimes ethnicity. For instance, if your total cholesterol level is 5.8 mmol/L and the reference range is listed as (< 5.0), it indicates that your cholesterol exceeds the recommended limit.
For haemoglobin, the reference range differs between men and women. Women typically fall between 115-165 g/L, while men range from 130-175 g/L. This explains why a result might be normal for one person but concerning for another.
Some results may fall into a "borderline" category. For example, an HbA1c result of 44 mmol/mol lies between the normal range (< 42 mmol/mol) and the diabetic range (≥ 48 mmol/mol). In such cases, your doctor might suggest monitoring or lifestyle adjustments rather than immediate treatment.
Flag symbols, such as 'H' for high or 'L' for low, highlight values outside the reference range. For example, a slightly elevated white blood cell count might just indicate your body is fighting off a minor infection.
UK Measurement Units Explained
Blood test reports in the UK use metric units, which may differ from those used in other countries. Here's a quick breakdown of the most common units:
- Millimoles per litre (mmol/L): Frequently used for measuring glucose, cholesterol, and electrolytes. This unit reflects the number of molecules in your blood, not their weight.
- Grams per litre (g/L): Used to measure protein levels, such as albumin or total protein, often in liver function or nutritional assessments.
- Units per litre (U/L): Common for enzyme levels, like ALT and AST (liver enzymes) or creatine kinase (muscle enzyme).
- Micrograms per litre (μg/L) and nanograms per millilitre (ng/mL): These measure very small concentrations, often used for substances like vitamin B12 or hormones.
- Nanomoles per litre (nmol/L): Used for vitamins like vitamin D. For instance, if your vitamin D levels increase from 25 nmol/L to 75 nmol/L after supplementation, you can clearly see the progress.
Understanding these units can help you track changes in your health over time.
What Doctor Comments Mean
Doctors often include comments in your lab report to provide context for your results. These comments are key to understanding what your numbers mean in relation to your health.
- "Within normal limits" or "normal": This means your results are comfortably within the reference range and no action is needed. These comments can be reassuring, especially if you're feeling anxious.
- "Abnormal": This simply indicates a result outside the normal range. It doesn't necessarily mean something serious but might require further monitoring or investigation. Your doctor will consider this alongside your symptoms and medical history.
- "Repeat test required" or "suggest repeat": This might appear if the results are inconsistent or if external factors, like not fasting properly, could have affected the outcome. It's usually a precaution rather than a cause for concern.
- Specific recommendations: Comments like "dietary advice recommended" for high cholesterol or "correlate results clinically" suggest next steps or emphasise the need to interpret results in the context of your overall health.
- Urgent or critical values: If your report includes terms like "telephoned to ward" or "critical result discussed with clinician", it means immediate action may be necessary. Your healthcare provider will contact you promptly to discuss what needs to be done.
Common Blood Test Markers Explained
Blood tests can reveal a lot about your health, offering a snapshot of your cardiovascular, metabolic, and general well-being. Here’s a breakdown of some key markers and what they mean.
Cholesterol Levels
A cholesterol panel is essential for assessing heart health. It includes several markers, each providing a piece of the puzzle.
- Total cholesterol gives an overall measure of cholesterol in your blood.
- HDL cholesterol (the "good" cholesterol) helps clear cholesterol from your arteries. Men should aim for levels above 1.0 mmol/L, and women above 1.2 mmol/L. Higher levels are linked to a lower risk of heart disease.
- LDL cholesterol (the "bad" cholesterol) can build up in your arteries, increasing the risk of heart disease. NHS guidelines recommend keeping LDL below 3.0 mmol/L, though for those with heart disease or diabetes, targets are as low as 1.8–1.4 mmol/L.
- Triglycerides measure fat in your blood. Levels above 2.3 mmol/L can indicate issues with fat metabolism, often linked to diet, alcohol, or conditions like diabetes. If triglycerides are high but other cholesterol levels are fine, lifestyle changes are usually the first step.
- The cholesterol ratio (total cholesterol divided by HDL) offers another perspective on cardiovascular risk. A ratio above 6 suggests increased risk, while below 4 is ideal.
Blood Sugar and HbA1c
These markers help evaluate how well your body manages sugar, both short and long term.
- Fasting glucose: A level below 6.0 mmol/L is normal. Ranges of 6.1–6.9 mmol/L indicate pre-diabetes, and 7.0 mmol/L or higher (on two occasions) suggests diabetes.
- Random glucose: If measured without fasting, levels above 11.1 mmol/L may indicate diabetes, especially if accompanied by symptoms like excessive thirst or frequent urination.
- HbA1c: This test reflects your average blood sugar over 2–3 months. Normal levels are below 42 mmol/mol, pre-diabetes falls between 42–47 mmol/mol, and diabetes is diagnosed at 48 mmol/mol or higher. For those managing diabetes, a target below 53 mmol/mol (7%) is common.
HbA1c is particularly useful as it isn’t influenced by meals prior to the test.
Haemoglobin and Full Blood Count (FBC)
A Full Blood Count provides vital details about your blood cells, helping diagnose conditions like anaemia, infections, and blood disorders.
- Haemoglobin carries oxygen in your blood. Low levels (below 120 g/L for women, 130 g/L for men) suggest anaemia, which can cause fatigue and breathlessness. High levels might point to dehydration or, less commonly, blood disorders.
- Red blood cell count: This works with haemoglobin. The MCV (mean cell volume) indicates the size of your red blood cells. Large cells might signal B12 or folate deficiency, while small cells could point to iron deficiency.
- White blood cell count: Normal levels range from 4.0–11.0 × 10⁹/L. High counts often mean your body is fighting an infection, while low counts may suggest immune issues or medication effects.
- Platelet count: A healthy range is 150–450 × 10⁹/L. Low platelets increase bleeding risk, while high levels may raise the risk of blood clots.
- Neutrophil percentage: This is a key part of your white blood cells. High neutrophils often indicate bacterial infections, while high lymphocytes might point to viral infections.
Liver and Kidney Function Tests
These tests assess how well your liver and kidneys are working.
- ALT (alanine aminotransferase) and AST (aspartate aminotransferase): These enzymes are released when liver cells are damaged. Normal ALT levels are below 40 U/L for men and 32 U/L for women. Elevated levels may signal liver inflammation from alcohol, medications, or viral hepatitis.
- ALP (alkaline phosphatase): High levels can point to liver or bone issues. GGT (gamma-glutamyl transferase) is particularly sensitive to alcohol and certain medications.
- Bilirubin: This measures waste from broken-down red blood cells. High levels can cause jaundice and may indicate liver problems or excessive red blood cell breakdown.
For kidney health:
- Creatinine: Normal levels are 60–110 μmol/L for women and 70–120 μmol/L for men. However, the eGFR (estimated glomerular filtration rate) is more telling, as it accounts for age, sex, and ethnicity. An eGFR above 90 mL/min/1.73m² is normal, while below 60 suggests chronic kidney disease.
- Urea: This waste product rises when kidney function declines but can also be affected by dehydration or a high-protein diet.
Vitamin and Hormone Levels
These markers provide insights into nutritional status and hormonal balance.
- Vitamin D: Measured in nmol/L in the UK. Levels below 25 nmol/L indicate severe deficiency, 25–50 nmol/L shows deficiency, and levels above 50 nmol/L are considered sufficient. Many people in the UK have low levels, especially in winter.
- Vitamin B12: Levels should be above 150 ng/L, though some experts recommend above 300 ng/L for optimal health. Low B12 can cause fatigue, nerve issues, and a specific type of anaemia with large red blood cells.
- Folate: This works with B12 and should be above 3.0 μg/L. Deficiency can lead to anaemia and is particularly important for women planning pregnancy.
- TSH (thyroid stimulating hormone): Normal levels range from 0.5–5.0 mU/L, though many doctors prefer 1.0–3.0 mU/L. High TSH suggests an underactive thyroid, while low TSH might indicate an overactive thyroid.
- Free T4: This measures active thyroid hormone. Levels should be in the upper half of the reference range (typically 10–25 pmol/L). Low T4 with high TSH confirms hypothyroidism, while high T4 with low TSH suggests hyperthyroidism.
- Ferritin: This measures iron stores. Levels below 15 μg/L indicate iron deficiency, even before anaemia develops. However, ferritin can be elevated in cases of inflammation, so it’s interpreted alongside other markers.
How to Read Your Results Step by Step
Once you've familiarised yourself with the components of your report, you can follow these steps to make sense of your blood test results.
Check Your Results Against Normal Ranges
Start by comparing your results to the reference ranges provided on your lab report. These ranges typically represent the middle 95% of results from healthy individuals and indicate what's considered normal for each test.
It's important to use the ranges specific to your lab, as different testing methods can produce slightly different values. Take note of where your result sits within the range. For example, a potassium level of 4.4 mmol/L within a reference range of 3.5–5.1 mmol/L is comfortably in the middle, suggesting normal kidney function and electrolyte balance. On the other hand, a cholesterol reading of 6.2 mmol/L compared to a range of 3.0–5.2 mmol/L exceeds the upper limit and may require attention.
Pay attention to how far your results deviate from the normal range. Significant deviations often need further investigation, while slight variations may just reflect normal fluctuations.
From here, consider how your personal circumstances might influence these numbers.
Think About Your Personal Situation
Your results should always be viewed in the context of your unique situation, as various factors can affect their meaning.
Age and gender play a key role in determining normal values. For instance, creatinine levels differ between men and women. Medications and supplements you're taking can also impact your results, so keep these in mind. Additionally, lifestyle factors - like whether you followed fasting instructions, exercised intensely the day before, or consumed alcohol - can temporarily affect markers such as triglycerides and glucose.
If you have any pre-existing conditions, this could alter how you interpret your results. For example, individuals managing chronic conditions may have different target ranges than the general population. Similarly, pregnancy can significantly change blood chemistry, meaning pregnancy-specific reference ranges are often applied.
After accounting for these factors, you can identify any results that may need immediate attention.
How to Talk to Your Doctor About Your Results
When discussing your blood test results with your doctor, it's essential to ask clear and specific questions. This helps you better understand the findings and their impact on your health. After reviewing your report, consider these key questions to make the most of your appointment.
Questions to Ask Your Doctor
- Is there anything unusual or abnormal about the result?
- What do these results mean for my overall health?
- What should I understand if my result is outside the reference range?
- Does a normal result mean there’s nothing to worry about?
- Does an abnormal result suggest a serious health concern?
These questions can help you navigate the conversation, ensuring you leave with a clear understanding of your results and any next steps.
How to Monitor Your Health Over Time
Keeping an eye on your blood test trends over time can reveal important changes in your health and how your body responds to lifestyle shifts or treatments. Let’s look at some practical ways to track and review these trends effectively.
Keep Track of Changes Over Time
Health isn’t just about one-off test results; it’s about patterns. To get a clear picture, maintain a simple health record. Include the dates of your tests, key results, and any major life changes - like starting new medications, altering your diet, or beginning an exercise routine.
Focus on tracking essential biomarkers. For heart health, this might include total cholesterol, LDL, HDL, and triglycerides. For diabetes, glucose and HbA1c are key metrics. Pair these with other relevant data, like your weight or blood pressure, to see the bigger picture.
It’s also helpful to note significant life events that might affect your results. For example, starting hormone therapy, experiencing menopause, or going through a particularly stressful period can all impact your biomarkers. This extra context can help both you and your doctor understand why certain numbers may fluctuate.
Don’t overlook seasonal patterns either. In the UK, vitamin D levels often drop during winter due to reduced sunlight, while cholesterol levels or weight might shift during festive seasons or summer holidays due to changes in eating and activity habits.
Set Health Goals Based on Your Results
Once you’ve got a system in place, use your blood test data to set clear, measurable health goals. Instead of vague objectives, work with your doctor to create specific targets based on your results.
For instance, if your LDL cholesterol is 4.2 mmol/L but should be below 3.0 mmol/L, discuss a plan with your GP. This might involve dietary changes and follow-up tests every three months to monitor progress.
Similarly, if your HbA1c is 7.5% and your doctor advises lowering it to below 7.0%, you can track improvements through regular testing while making lifestyle adjustments.
Celebrate your progress. Watching your vitamin D levels rise from deficient to optimal or seeing liver function markers improve after cutting down on alcohol can be incredibly motivating. These tangible improvements reinforce the benefits of sticking to healthy habits.
Keep in mind that different biomarkers respond at different speeds. Cholesterol levels might improve within 6-8 weeks of dietary changes, while HbA1c requires patience, reflecting average blood sugar over the past 2-3 months. Stick with it, and the results will follow.
Take Control of Your Health with Epsom Blood Tests
Understanding your blood test results is an important step, but having clear, expert-reviewed reports takes it to the next level. Instead of waiting for a GP appointment to decipher what your numbers mean, Epsom Blood Tests provides immediate clarity. Their doctor-reviewed reports don’t just present data - they explain it in plain English, so you can take meaningful action for your health.
Epsom Blood Tests redefines the blood testing experience. Each report includes detailed commentary from qualified doctors, highlighting key findings and offering clear next steps.
"Results are presented in clear visuals, not confusing numbers"
"Anything unusual is highlighted with comments and next steps"
"So you get clarity, confidence, and a plan for your health"
What sets Epsom Blood Tests apart is their personalised approach. Instead of relying on generic reference ranges, the reports are tailored to your individual health profile. For example, if your cholesterol levels are slightly high, the analysis will not only flag it but explain its potential impact on your heart health and suggest specific lifestyle changes. Similarly, if a vitamin deficiency is detected, you’ll receive actionable advice rather than vague suggestions. This level of detail ensures the guidance is relevant and practical.
"With expert analysis, you'll get a personalised roadmap to better health, empowering you to make informed decisions."
Beyond the insights, the service offers convenience. Reports are delivered securely and digitally, allowing you to access them anytime, anywhere. This makes it easy to track progress over time, whether you're monitoring cholesterol levels or keeping tabs on vitamins and hormones. The seamless access integrates smoothly into your ongoing health management.
With over 3,250 excellent reviews on Trustpilot and a 4.9-star rating from more than 300 Google reviews, Epsom Blood Tests has earned its reputation for helping people understand and act on their health data. By combining detailed testing with expert interpretation and straightforward communication, they provide more than just results - they give you the tools to take control of your health.
FAQs
What does it mean if my blood test results are borderline?
Borderline blood test results indicate that your values are just outside the normal range, but not by a large margin. This usually isn’t a reason to panic, as it can often be linked to temporary factors like what you’ve eaten recently, stress levels, or small natural changes in your body.
Doctors don’t look at these results in isolation - they consider them alongside your overall health, medical history, and other test results. Often, no immediate action is required unless there are other symptoms or risk factors present. If you’re feeling uncertain, it’s always a good idea to talk to your healthcare provider to better understand what these results mean for you.
What should I do if my blood test results are outside the normal range but I haven’t heard from my doctor?
If your blood test results are outside the normal range and your doctor hasn’t contacted you, it’s wise to get in touch with your GP or healthcare provider. While not all results demand urgent attention, it’s always worth understanding their significance - particularly if you’re feeling unwell or have specific concerns.
Keep in mind that slightly unusual results aren’t always a cause for alarm. However, speaking with your healthcare provider can help determine if additional tests or follow-up actions might be necessary.
How do diet and exercise affect blood test results, and what changes can help improve them?
Your diet and exercise habits play a key role in shaping your blood test results. Regular physical activity can help lower cholesterol, regulate blood sugar, and support heart health. Meanwhile, a diet rich in fruits, vegetables, lean proteins, and whole grains contributes to maintaining healthy cholesterol and blood glucose levels. On the flip side, consuming processed foods, too much salt, or not staying hydrated can skew your results in the wrong direction.
If you want to get the best outcomes from your blood tests, focus on maintaining a healthy weight, drink plenty of water, and avoid intense exercise right before your test, as it might temporarily affect some readings. Building consistent habits, like cutting back on saturated fats and including moderate exercise in your routine, can bring about lasting improvements in your health markers.
